Xyplorer Scripts Express Members
2020 Express Scripts National Preferred Formulary List The 2020 National Preferred Formulary drug list is shown below. The formulary is the list of drugs included in your prescription plan.
Types of pharmacies
Preferred home delivery from Express Scripts Pharmacy®

If you take prescription drugs every day or on a regular basis, consider the added safety, convenient service and potential savings of having a 90-day supply delivered right to your mailbox.
- Low costs. Receive up to a 90-day supply of your medication for a low copay or coinsurance.
- Added safety and convenience. We mail directly to your home so you can avoid making trips and waiting in line at the pharmacy. Medications typically arrive within 10 days after we receive the prescription from your doctor.
- Free standard shipping. We include shipping as part of your plan at no additional cost.
- 24/7 care and service. Express Scripts pharmacists are available by phone to answer your medication questions, even in the middle of the night.
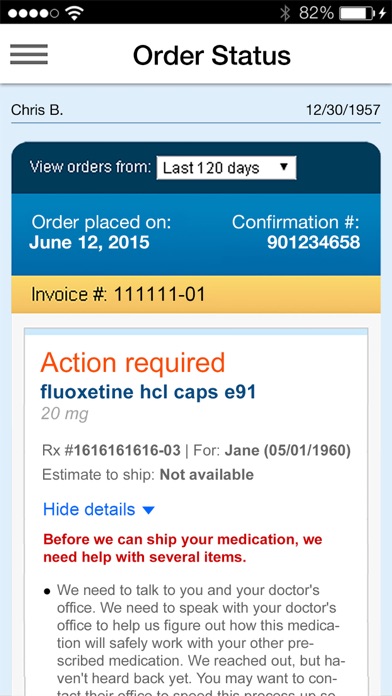
- Easy refills. On our website, with the Express Scripts® mobile app, by phone or by mail.
- Apr 06, 2020 Express Scripts will make SilverCloud Health’s digital behavioral health platform available for free to its members as they navigate the COVID-19 pandemic.
- Oct 01, 2020 Drug Coverage. The Choice plan Medicare Part D Formulary (drug list) has more than 3,100 drugs, including the most commonly used medications. The Part D Senior Savings Model for our Choice plan offers Tier 6 select insulins for a $0 copay at a preferred pharmacy or $11 at a standard pharmacy for a 30-day supply in all stages up to the Catastrophic Coverage Stage.
Some medications, such as narcotics, cannot be filled through home delivery from Express Scripts Pharmacy®
Preferred retail pharmacies
Certain network pharmacies offer preferred cost-sharing for plan members. When you use one of our preferred pharmacies, you’ll typically pay less for your drugs than when you use a pharmacy with standard cost-sharing.
| Saver plan | Value plan | Choice plan |
| CVS Pharmacy® Walmart | Walgreens Walmart | Walgreens + Local, Independent Pharmacies |
Dillons, Fred Meyer, Fry's, Harris Teeter, King Soopers, Mariano's, Metro Market, Pick 'n Save, QFC, Ralphs, Smith's | ||
To transfer a prescription to a preferred retail pharmacy, ask the preferred pharmacy to contact your current pharmacy to transfer any remaining refills. Or, you can wait until you receive a new prescription and ask your doctor to submit it to a preferred pharmacy.
Standard retail pharmacies
Our standard retail pharmacy network includes national drug and grocery stores, so you can be confident that you'll have convenient access to the medicines you need, whether you’re at home or traveling anywhere in the U.S. You can confirm whether your pharmacy is preferred or standard using our online searchable directory.

To request a Pharmacy Directory be mailed to you, send an email with your full name, phone number and mailing address to documents@express-scripts.com. For assistance, call 1.866.477.5703, 8 a.m. to 8 p.m., 7 days a week, except Thanksgiving and Christmas. Fastboot drivers for windows 10. TTY users, call 1.800.716.3231.
In most cases, your prescriptions are covered by Express Scripts Medicare only if they are filled at a network pharmacy or through home delivery. The plan will fill prescriptions at out-of-network pharmacies under certain circumstances as described in our Evidence of Coverage.
Other pharmacies are available in our network.
If you qualify for Extra Help from Medicare to pay for your prescription drug costs, the amounts listed here may not apply to you.
Medicare Part B prescription drugs are not covered under the prescription drug benefit (Part D). Generally, we cover only prescription drugs, vaccines, biological products and medical supplies that are covered under the Medicare prescription drug benefit (Part D) and that are on our formulary.
Xyplorer Scripts Express Members Sign In Page
Express Scripts Medicare’s pharmacy network includes limited lower-cost, preferred pharmacies in rural areas in Alaska; the Saver plan also includes limited lower-cost, preferred pharmacies in suburban areas in Puerto Rico, and the Choice plan also includes limited lower-cost, preferred pharmacies in rural areas in Oklahoma. The lower costs advertised in our plan materials for these pharmacies may not be available at the pharmacy you use. For up-to-date information about our network pharmacies, including whether there are any lower-cost preferred pharmacies in your area, please call Customer Service at 1.866.477.5703; TTY: 1.800.716.3231, or consult the online pharmacy directory.
Certain prescription drugs will have maximum quantity limits.
Xyplorer Scripts Express Members Directory
Your prescriber must get prior authorization from Express Scripts Medicare for certain prescription drugs.

Covered Part D drugs are available at out-of-network pharmacies under certain circumstances, including illness while traveling outside the plan's service area, where there is no network pharmacy. You may also incur an additional cost for drugs received at an out-of-network pharmacy.
We have free interpreter services available to answer any questions you may have about the plan.
View information on multi-language interpreter services.
